Dental Bone Graft Risks and Benefits: What Patients Should Know
Introduction
Dental bone grafting is a common procedure often recommended when patients need additional bone to support dental implants, treat periodontal disease, or restore bone loss due to trauma or tooth extraction. Understanding the benefits and risks of bone grafting is essential for anyone considering the procedure.
Definition
Dental bone grafting is a surgical procedure that uses synthetic, natural, or artificial replacements to replace or join missing or damaged body components. These grafting procedures are useful in treating bony abnormalities brought on by disease, trauma, or resorption. Dental fillers are made from bone transplants. The grafting process can help with bone healing as well as bone formation. The oral bone transplant provides a biodegradable antibody response. It serves as a mineral storage by growing new bone.
What is a Dental Bone Graft?
A dental bone graft is a surgical procedure that involves transplanting bone material to areas where the jawbone has deteriorated or is insufficient. The purpose is to stimulate the growth of new bone, which can provide a stable foundation for dental implants or other restorative procedures. Over time, the graft integrates with the existing bone, creating a solid structure for tooth replacement.
In dental operations, bone transplants are mostly employed in four types:
- Autografts: Bone is taken from the patient’s own body, usually from the chin, jaw, or another area.
- Allografts: Human donors provide bone material, usually obtained through a bone bank.
- Xenografts: Bone is derived from an animal, often bovine (cow), which is processed and sterilized before use.
- Alloplasts: Natural bone is replaced by synthetic bone material, such as calcium phosphate.
Each type of graft has its pros and cons, and the choice of graft depends on the patient’s specific needs, medical history, and the recommendation of their dental surgeon.
Benefits of Dental Bone Grafts
Dental bone grafting offers several advantages, particularly for patients planning dental implants or those with significant bone loss. Here are some key benefits:
1. Improved Dental Implant Success
One of the primary reasons for bone grafting is to ensure that patients can receive dental implants. In order to firmly anchor the titanium post in an implant, enough bone must exist. If a patient’s jawbone has atrophied, there may not be enough material to support the implant. Bone grafting can provide the necessary foundation, increasing the likelihood of a successful implant procedure.
2. Preserving Facial Structure
When teeth are lost, the jawbone can begin to resorb or shrink, which can affect the overall structure of the face. This loss of bone can cause a sunken or prematurely aged appearance. Bone grafts help maintain or restore the shape of the jawline, preserving facial aesthetics and preventing further bone loss.
3. Supporting Gum Health
Patients suffering from periodontal disease may experience bone loss around the teeth, which can destabilize the teeth and cause them to shift or loosen. Bone grafting, in conjunction with other periodontal treatments, can restore lost bone, stabilize teeth, and promote healthier gums, ultimately supporting better oral health.
4. Restoring Functionality
In cases where trauma, infection, or other conditions have led to bone loss, patients may have difficulty chewing, speaking, or maintaining a proper bite. Bone grafting can restore the jaw’s structural integrity, allowing patients to regain full functionality of their mouth.
5. Preventing Further Bone Loss
Bone grafts not only replace missing bone but also stimulate the growth of new bone tissue. This regeneration helps to prevent further bone loss in the affected area, ensuring long-term oral health.
Risks of Dental Bone Grafts
While dental bone grafting is generally safe and has a high success rate, it’s important to be aware of the potential risks and complications associated with the procedure. Patients should discuss these risks with their dental surgeon before undergoing the procedure. Here are some of the most common risks:
1. Infection:
As with any surgical procedure, there is a risk of infection after a dental bone graft. Infections can occur if bacteria enter the surgical site, leading to pain, swelling, and in severe cases, the failure of the graft. To minimize this risk, dentists prescribe antibiotics and provide instructions on how to keep the area clean.
2. Graft Rejection or Failure:
In some cases, the body may reject the graft material, especially when using allografts, xenografts, or alloplasts. If the graft fails to integrate with the patient’s existing bone, it may need to be removed or replaced. Autografts have the lowest risk of rejection since the bone is harvested from the patient’s own body.
3. Bleeding and Swelling:
After the procedure, patients can experience some bleeding, swelling, and discomfort around the graft site. While this is usually temporary and can be managed with pain medication and cold compresses, excessive bleeding or swelling may require further medical attention.
4. Nerve Damage:
There is a risk of nerve damage, particularly in the lower jaw, where nerves are located close to the bone. Nerve damage can result in numbness, tingling, or pain in the lips, chin, or tongue. While this complication is rare, it can sometimes be permanent, so surgeons take precautions to avoid this risk.
5. Prolonged Healing Time:
Bone grafting can have a longer recovery period compared to other dental procedures. Depending on the extent of the graft and the patient’s overall health, it can take several months for the graft to fully integrate with the existing bone. Patients must follow their dentist’s post-operative care instructions carefully to ensure proper healing.
6. Complications with Sinus Lifting:
For patients requiring bone grafts in the upper jaw, a sinus lift may be necessary to create enough space for the graft material. While generally safe, this procedure carries its own risks, including sinus infections or perforation of the sinus membrane.
What to Expect During and After the Procedure
Understanding the procedure and recovery process can help alleviate anxiety and ensure a smoother experience for patients. Here’s what to expect:
During the Procedure
Dental bone grafting is typically performed under local anesthesia, though sedation may be used for patients who are anxious or undergoing more complex procedures. The dentist will make an incision in the gum to expose the bone and then place the graft material in the desired area. The site is then closed with stitches, and a protective dressing may be applied.
Recovery and Aftercare
Following the procedure, patients will be given specific instructions on how to care for the surgical site. For a few days, pain and swelling are typical; to treat discomfort and avoid infection, dentists frequently recommend painkillers and antibiotics. Patients should abstain from smoking, heavy lifting, and meals that could cause discomfort at the graft site.
Depending on the patient’s condition and the amount of the transplant, full recovery may take three to nine months. During this time, follow-up appointments will be necessary to monitor the progress of the healing and to determine when it’s safe to proceed with the next phase of treatment, such as dental implants.
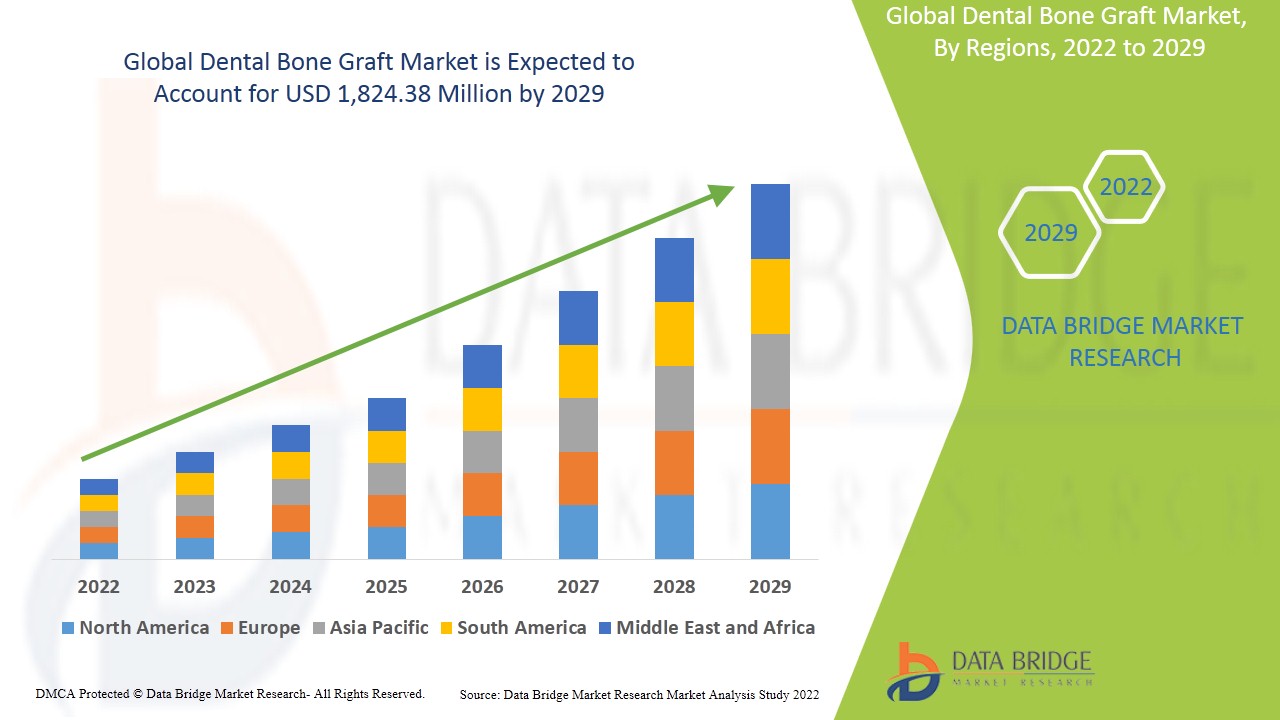
Growth Rate of Dental Bone Graft Market
The dental bone graft market is predicted to reach USD 2284.41 million by 2031, growing at a compound annual growth rate (CAGR) of 11.90% from 2024 to 2024, when it was estimated to be worth USD 929.25 million in 2023.
Read More: https://www.databridgemarketresearch.com/reports/global-dental-bone-graft-market
Conclusion
Dental bone grafting offers significant benefits for patients dealing with bone loss, whether due to trauma, periodontal disease, or preparation for dental implants. The procedure can restore the structure and function of the jawbone, prevent further bone loss, and support long-term oral health. However, like any surgery, it carries risks such as infection, graft failure, and prolonged healing. Patients should discuss these risks and benefits with their dentist to make an informed decision tailored to their unique oral health needs.